6 Natural Remedies for Managing Ulcerative Colitis (UC)
Table of Contents
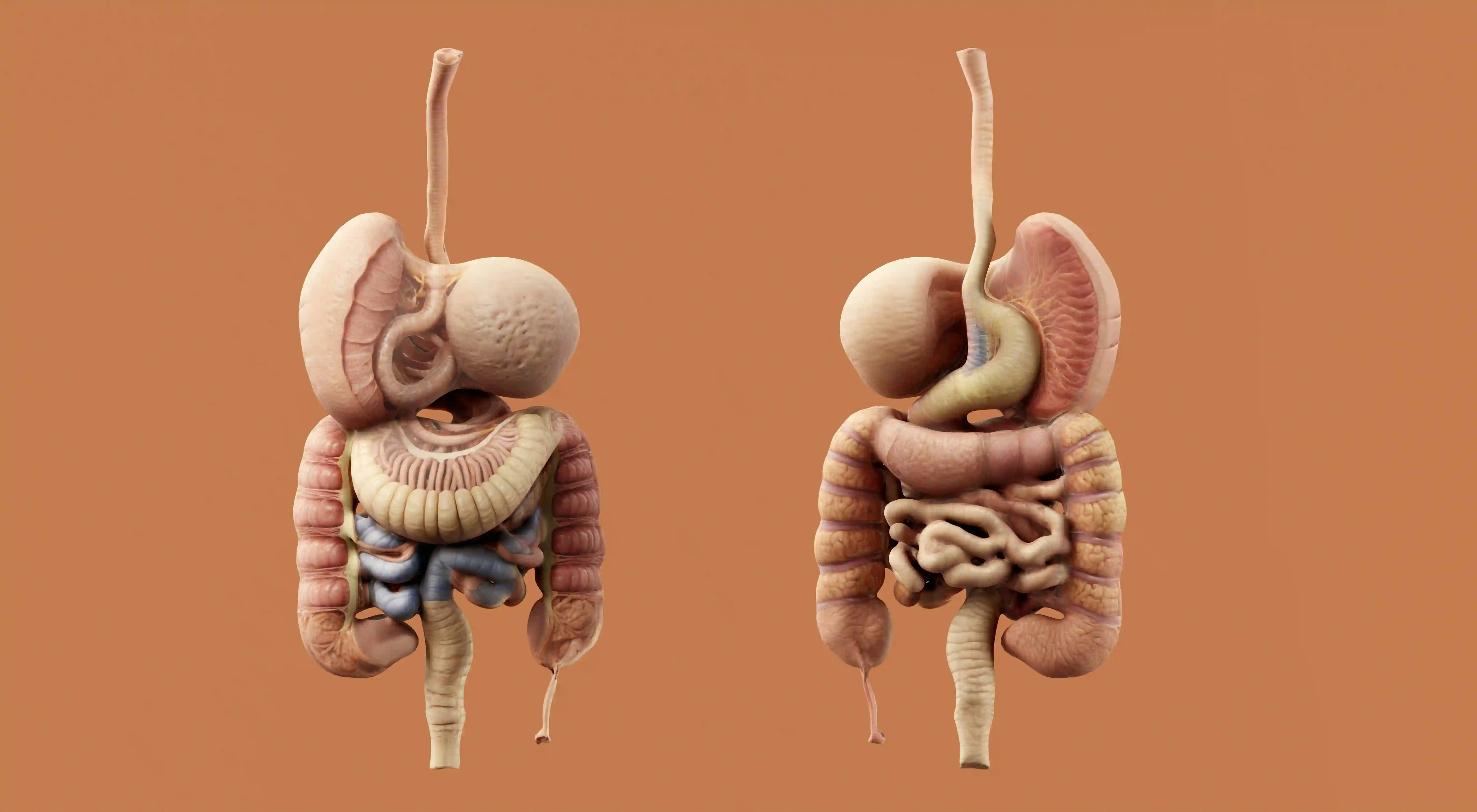
Ulcerative colitis is a chronic inflammatory bowel disease that affects the lining of the colon and rectum. While medical treatment remains the cornerstone of care, many people explore natural remedies to complement prescribed therapy. These approaches aim to reduce inflammation, improve gut health, and enhance overall quality of life when used responsibly.
-
Diet
Diet plays a critical role in managing ulcerative colitis symptoms, particularly during flare ups. While no single diet works for everyone, many people find symptom relief by avoiding foods that irritate the digestive tract or worsen inflammation.
During active disease, bland and easily digestible foods such as rice, bananas, eggs, and well cooked vegetables are often better tolerated. High fiber foods may worsen symptoms during flares, although soluble fiber can sometimes be helpful during remission.
Keeping a food diary can help identify individual triggers such as dairy products, spicy foods, alcohol, or high fat meals. Adequate nutrition is essential, as ulcerative colitis can increase the risk of deficiencies in iron, calcium, vitamin D, and protein.
-
Herbal remedies
Certain herbal remedies have been studied for their potential anti inflammatory effects in ulcerative colitis. These remedies are not replacements for medication but may offer additional symptom support for some individuals.
Turmeric, which contains the active compound curcumin, has shown promise in reducing intestinal inflammation when used alongside standard therapy. Aloe vera gel has also been explored for its soothing effects on the gut lining.
Herbal treatments should always be discussed with a healthcare provider before use. Some herbs can interact with medications or cause side effects, especially when taken in high doses or for extended periods.
-
Probiotics
Probiotics are beneficial bacteria that help maintain balance within the gut microbiome. In ulcerative colitis, this balance is often disrupted, contributing to inflammation and symptoms.
Certain probiotic strains may help reduce symptoms and prolong remission by supporting the intestinal barrier and modulating immune responses. Fermented foods such as yogurt with live cultures, kefir, and fermented vegetables are natural sources of probiotics.
Not all probiotics work the same way, and effectiveness can vary between individuals. Consistent use over several weeks is often necessary before any benefits are noticed.
-
Exercise
Regular physical activity offers benefits beyond general fitness for people with ulcerative colitis. Exercise can help reduce inflammation, improve mood, and support immune system regulation.
Low to moderate intensity activities such as walking, swimming, yoga, and cycling are generally well tolerated. These activities can help reduce fatigue and support bowel regularity without placing excessive strain on the body.
During flare ups, exercise intensity may need to be reduced. Listening to the body's signals and prioritizing rest during active disease is an important part of long term management.
-
Stress
Psychological stress does not cause ulcerative colitis, but it can significantly worsen symptoms and trigger flare ups. Stress activates pathways that influence gut inflammation and intestinal motility.
Stress management techniques such as mindfulness meditation, deep breathing exercises, and progressive muscle relaxation may help reduce symptom severity. Cognitive behavioral therapy has also shown benefit in improving coping skills.
Adequate sleep, social support, and realistic daily routines contribute to emotional wellbeing. Many individuals report fewer symptoms when stress levels are consistently managed.
-
Acupuncture
Acupuncture is a traditional therapy that involves inserting thin needles into specific points on the body. It is believed to influence nervous system pathways and reduce inflammation.
Some people with ulcerative colitis report improvements in abdominal pain, bowel frequency, and stress levels after acupuncture sessions. Benefits may be related to improved pain modulation and relaxation.
While evidence is still emerging, acupuncture is generally considered safe when performed by trained professionals. It should be viewed as a complementary approach rather than a standalone treatment.
Takeaway
Natural remedies can play a supportive role in managing ulcerative colitis when combined with appropriate medical care. Approaches such as dietary modification, stress reduction, and gut focused therapies aim to improve daily comfort and long term wellbeing.
It is important to remember that ulcerative colitis is a chronic condition that requires ongoing monitoring. Any new remedy should be discussed with a healthcare professional to ensure safety and effectiveness.
Frequently Asked Questions about Ulcerative Colitis
Can natural remedies replace medication for ulcerative colitis?
Natural remedies should not replace prescribed medication for ulcerative colitis. Medical therapy is essential for controlling inflammation and preventing complications.
Natural approaches are best used as complementary strategies alongside medical treatment, under guidance from a qualified healthcare provider.
Are natural remedies safe during flare ups?
Some natural remedies may be helpful during flare ups, but others can worsen symptoms. Individual tolerance varies widely among people with ulcerative colitis.
It is important to introduce any new remedy cautiously and seek medical advice, especially during periods of active disease.
How long does it take to see benefits from natural remedies?
The time required to notice benefits varies depending on the remedy and the individual. Some people notice changes within weeks, while others require longer periods.
Consistency and realistic expectations are important, as natural approaches often provide gradual rather than immediate improvement.
Can diet alone control ulcerative colitis?
Diet can significantly influence symptoms, but it usually cannot control ulcerative colitis on its own. Inflammation often persists without medical treatment.
A balanced dietary approach combined with medication offers the best chance of maintaining remission and preventing disease progression.
How we reviewed this article:
Our team continually monitors and updates articles whenever new information becomes available.
Written By
Ian Nathan, an MBChB Candidate, and the Healtharticles Editorial Team
Medically Reviewed By
Ian Nathan, an MBChB Candidate