Everything about IBS-D (Irritable Bowel Syndrome With Diarrhea)
Table of Contents
People with IBS-D experience frequent loose or watery stools, often accompanied by urgency and abdominal cramping. Symptoms may fluctuate over time, with periods of relative improvement followed by flare ups. Stress, certain foods, infections, and hormonal changes can worsen symptoms in susceptible individuals.

What is IBS-D (Irritable Bowel Syndrome With Diarrhea)
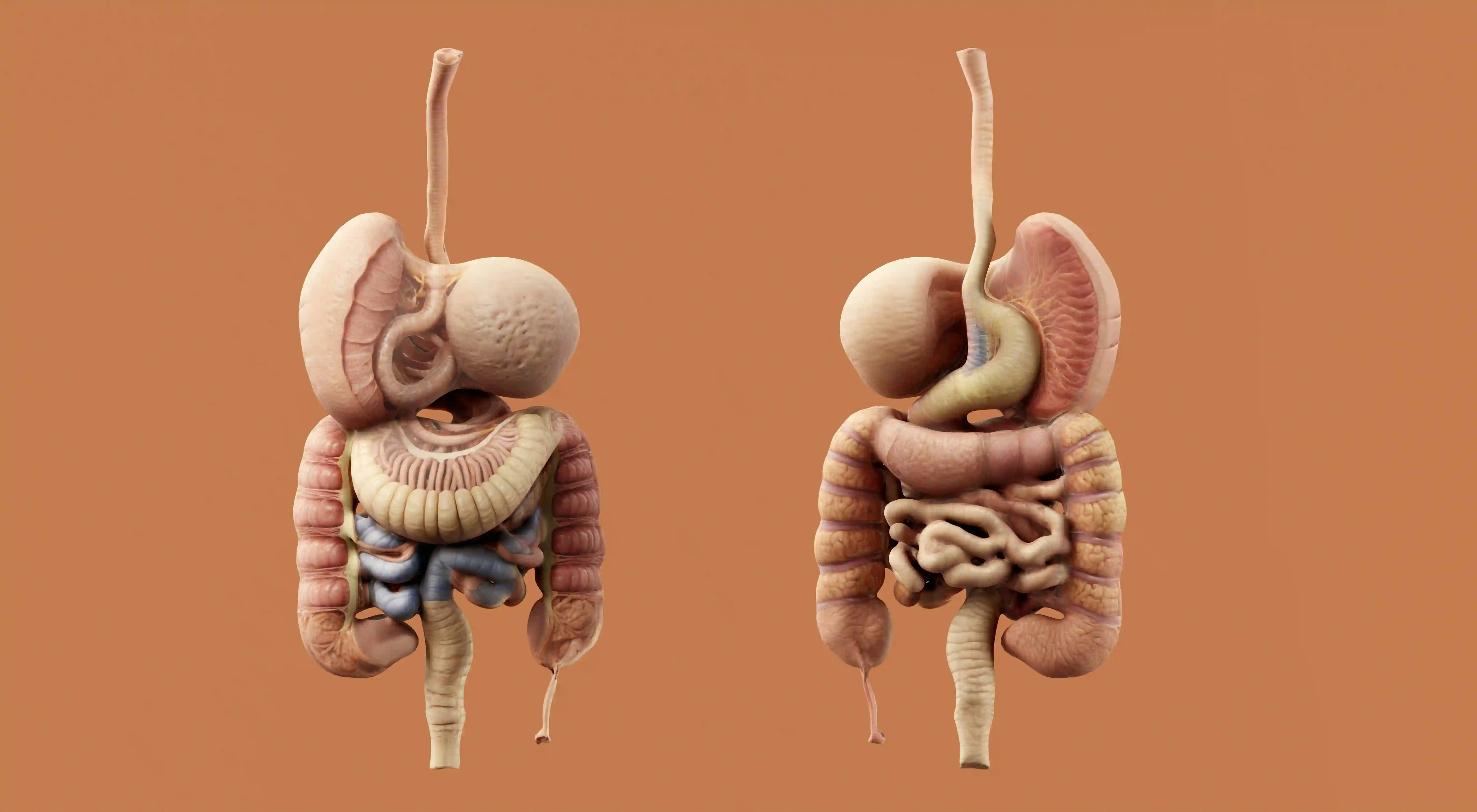
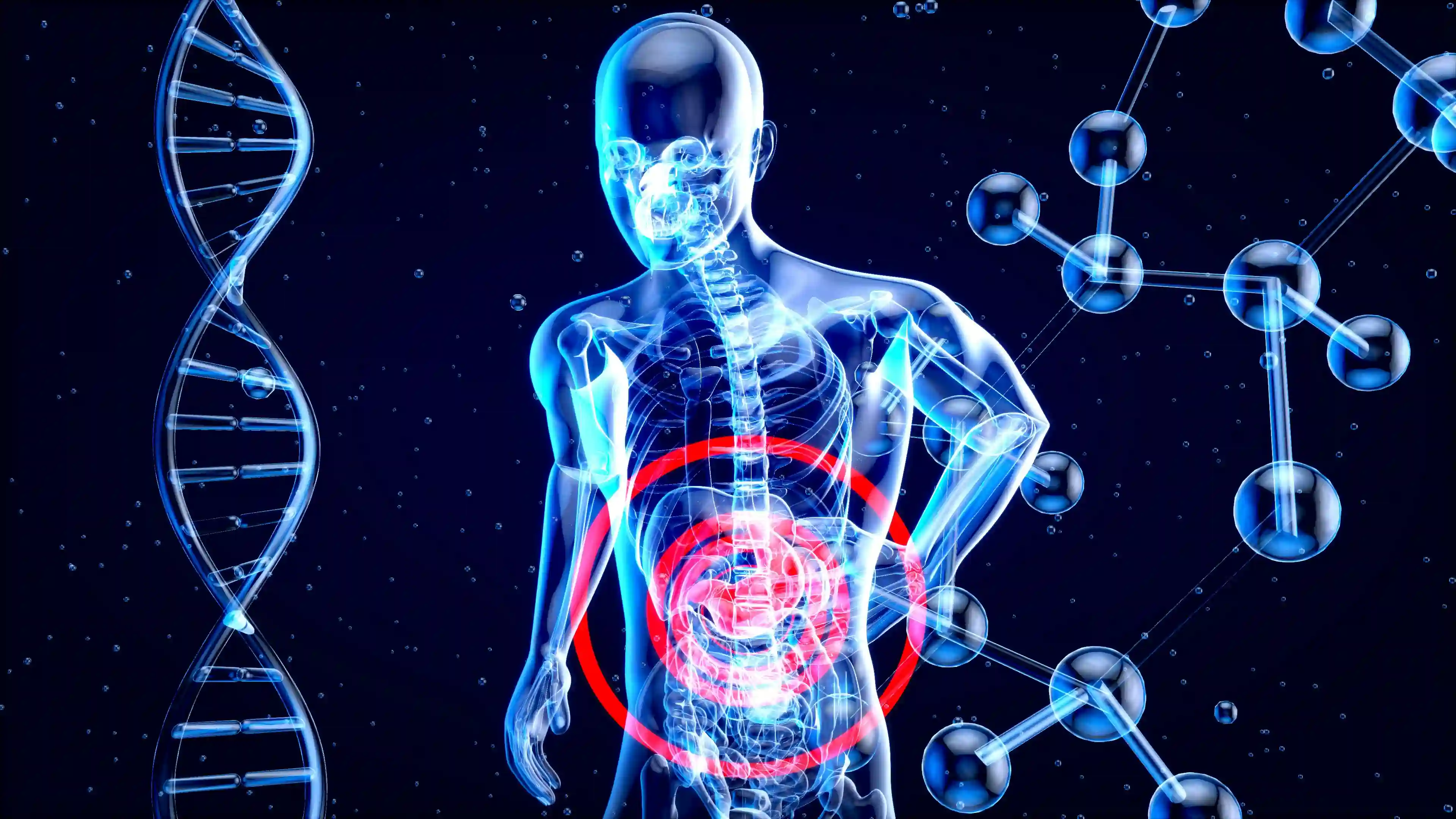
IBS-D is a subtype of irritable bowel syndrome characterized primarily by chronic or recurrent diarrhea along with abdominal discomfort. It is considered a functional gastrointestinal disorder, meaning symptoms occur without visible structural damage to the digestive tract. The condition affects how the gut and brain communicate, often referred to as the gut brain axis.
Although IBS-D does not cause permanent damage to the intestines or increase the risk of colorectal cancer, it can significantly affect quality of life. Many individuals report disruptions to work, social activities, and mental wellbeing due to unpredictable bowel habits.
Symptoms
The hallmark symptom of IBS-D is chronic diarrhea, typically defined as loose stools occurring more than once daily for several weeks or months. These episodes are often associated with abdominal pain that improves after passing stool. Stool consistency may vary, but urgency is a common complaint.
Other symptoms include bloating, excessive gas, and a sensation of incomplete bowel emptying. Mucus may be present in the stool, which can be alarming but is generally harmless in IBS-D. Symptoms often worsen after meals, especially large or high fat meals.
Extra intestinal symptoms are also common. These may include fatigue, sleep disturbances, anxiety, and difficulty concentrating. Many people notice that emotional stress directly worsens gastrointestinal symptoms, reinforcing the close link between the nervous system and the gut.
Diagnosis
IBS-D is diagnosed primarily based on clinical criteria rather than a single definitive test. Doctors often use the Rome IV criteria, which focus on recurrent abdominal pain associated with changes in stool frequency or form over at least three months.
A thorough medical history and physical examination are essential to rule out other causes of chronic diarrhea. Alarm features such as unintended weight loss, anemia, rectal bleeding, or symptoms beginning after age 50 usually prompt further investigation.
Tests may include blood work, stool studies, and sometimes colonoscopy to exclude infections, inflammatory bowel disease, celiac disease, or colorectal cancer. Once serious conditions are excluded, a diagnosis of IBS-D can usually be made with confidence.
Lifestyle
Lifestyle modification plays a central role in managing IBS-D. Stress reduction is particularly important, as psychological stress can intensify gut motility and pain perception. Techniques such as mindfulness, deep breathing exercises, and cognitive behavioral therapy have shown benefit in many patients.
Regular physical activity supports healthy digestion and stress control. Moderate exercise such as walking, cycling, or swimming for 20 - 40 minutes several times per week can improve bowel regularity and overall wellbeing without aggravating symptoms.
Sleep quality should not be overlooked. Poor sleep can worsen pain sensitivity and bowel symptoms. Establishing consistent sleep routines and aiming for 7 - 9 hours of rest each night may reduce symptom severity over time.
Diet
Dietary management is one of the most effective strategies for IBS-D symptom control. Many patients benefit from identifying and avoiding trigger foods that worsen diarrhea or bloating. Common triggers include caffeine, alcohol, spicy foods, and high fat meals.
The low FODMAP diet is frequently recommended under professional guidance. This approach reduces intake of fermentable carbohydrates that can increase gas production and water movement in the intestines. Foods are typically eliminated temporarily and then reintroduced gradually.
Adequate hydration is essential, especially for individuals experiencing frequent diarrhea. Soluble fiber sources such as oats, psyllium, and bananas may help improve stool consistency, whereas insoluble fiber can worsen symptoms in some people.
Medication
Medication may be required when lifestyle and dietary measures are insufficient. Treatment is usually tailored to the dominant symptoms and individual response. Anti diarrhea agents such as loperamide are commonly used to reduce stool frequency and urgency.
Antispasmodic medications can help relieve abdominal cramping by relaxing intestinal smooth muscle. In some patients, bile acid sequestrants are effective, particularly when diarrhea is driven by bile acid malabsorption.
For moderate to severe cases, prescription medications that target gut receptors or alter intestinal secretion may be considered. Low dose antidepressants are sometimes used to reduce pain perception and improve gut brain communication, even in patients without depression.
Takeaway
IBS-D is a chronic but manageable condition that affects the interaction between the gut and the nervous system. While symptoms can be disruptive, they do not indicate serious disease or long term intestinal damage.
Effective management often requires a combination of education, lifestyle modification, dietary changes, and medication when necessary. Working closely with a healthcare provider can help tailor treatment strategies to individual needs.
With proper support and a personalized approach, many people with IBS-D achieve significant symptom improvement and regain control over daily life.
Frequently Asked Questions about IBS-D
Is IBS-D the same as chronic diarrhea?
IBS-D is one cause of chronic diarrhea, but not all chronic diarrhea is IBS-D. The diagnosis depends on symptom patterns, abdominal pain, and exclusion of other medical conditions through appropriate evaluation.
Unlike many organic diseases, IBS-D does not involve inflammation or structural damage. Symptoms are related to altered gut function and sensitivity rather than infection or tissue injury.
Can stress really worsen IBS-D symptoms?
Stress plays a major role in IBS-D because the gut and brain communicate closely through neural and hormonal pathways. Emotional stress can increase bowel motility and pain sensitivity.
Many patients notice symptom flares during periods of anxiety or major life changes. Stress management techniques can therefore be an important part of treatment.
Is IBS-D a lifelong condition?
IBS-D is considered a chronic condition, but symptoms often fluctuate over time. Some individuals experience long periods of remission with minimal or no symptoms.
With appropriate management strategies, many people learn to control symptoms effectively and maintain a good quality of life over the long term.
Should everyone with IBS-D follow a low FODMAP diet?
Not everyone with IBS-D requires a low FODMAP diet. While it can be helpful, it should ideally be tried under the guidance of a trained healthcare professional.
Long term unnecessary restriction can lead to nutritional imbalance, so foods should be reintroduced gradually to identify personal triggers rather than avoiding entire groups permanently.
How we reviewed this article:
Our team continually monitors and updates articles whenever new information becomes available.
Written By
Ian Nathan, an MBChB Candidate, and the Healtharticles Editorial Team
Medically Reviewed By
Ian Nathan, an MBChB Candidate