Everything You Need to Know About Obsessive-Compulsive Personality Disorder (OCPD)
Table of Contents
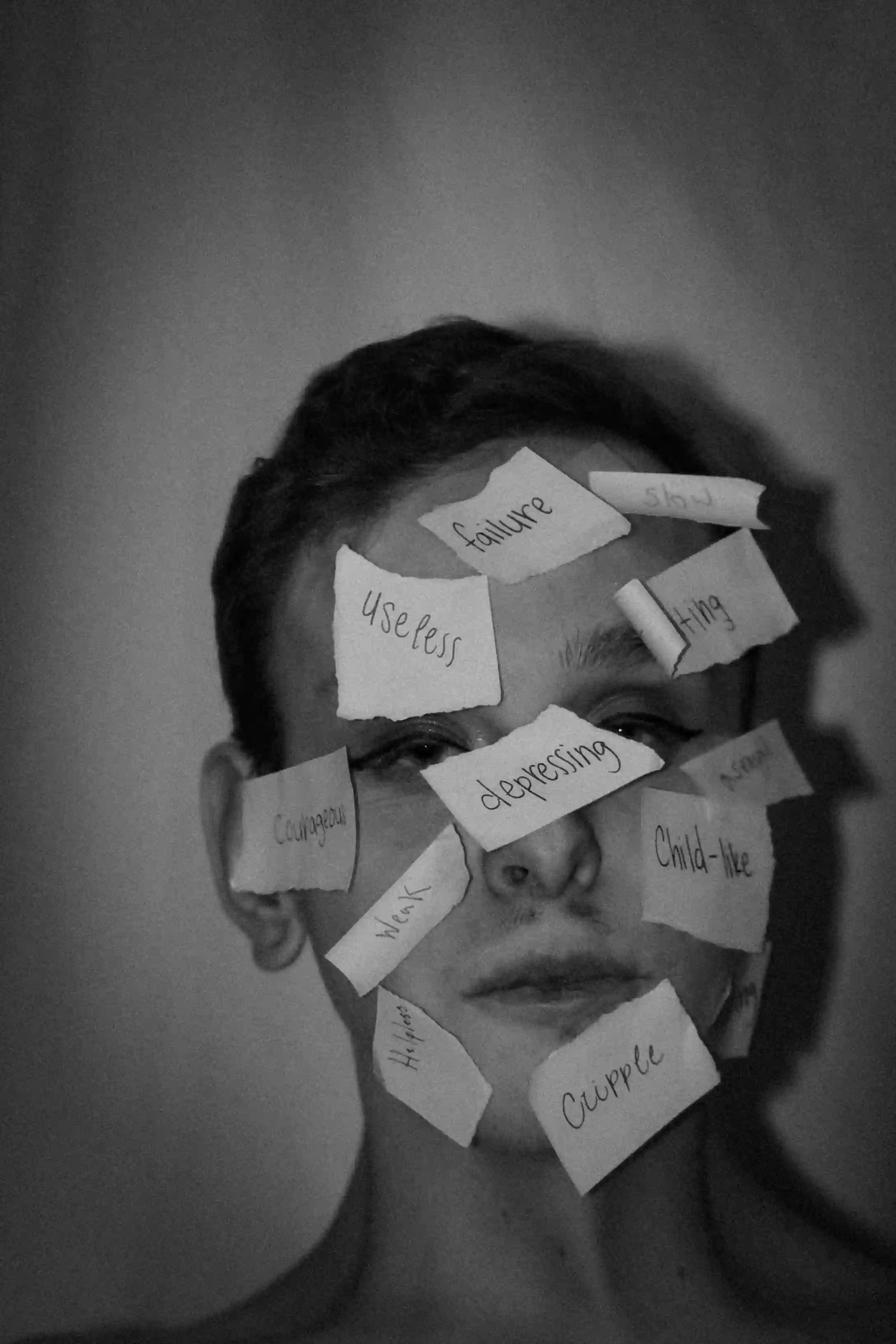
Obsessive-Compulsive Personality Disorder, commonly abbreviated as OCPD, is a personality disorder characterized by a pervasive pattern of orderliness, perfectionism, and control. Unlike obsessive-compulsive disorder (OCD), OCPD does not primarily involve intrusive thoughts or repetitive behaviors performed to reduce anxiety. Instead, the traits of OCPD are deeply ingrained and often viewed by the individual as appropriate or even superior.
People with OCPD may be highly dependable, detail-oriented, and committed to their work. However, these same traits can cause significant difficulties in relationships, flexibility, and emotional well-being. Understanding OCPD requires examining its causes, symptoms, and available support options.
Causes
The exact cause of OCPD is not fully understood, but research suggests it develops through a combination of biological, psychological, and environmental influences. No single factor is responsible, and the condition likely emerges gradually over time.
Genetic factors appear to play a role. Studies indicate that personality traits related to rigidity, conscientiousness, and perfectionism can run in families. This suggests a hereditary vulnerability that may increase the likelihood of developing OCPD.
Early life experiences are also important. Individuals raised in environments with strict rules, high expectations, or conditional approval may internalize rigid standards. Over time, these standards can become core personality features rather than adaptive behaviors.
Neurobiological theories suggest differences in brain regions involved in cognitive control and emotional regulation. While this area is still being studied, it may help explain why individuals with OCPD struggle with flexibility and emotional expression.
Risk factors
Certain factors increase the likelihood of developing OCPD, although their presence does not guarantee the disorder will occur.
Family history of personality disorders, anxiety disorders, or obsessive traits increases risk. Shared genetics and upbringing may both contribute.
Childhood environment plays a significant role. Risk is higher in individuals who experienced:
- Excessive emphasis on rules or discipline
- Limited emotional warmth or validation
- Harsh punishment for mistakes
Temperamental traits such as high conscientiousness, low tolerance for uncertainty, and discomfort with emotional expression may predispose someone to OCPD when combined with environmental stressors.
Symptoms
Symptoms of OCPD typically begin by early adulthood and remain relatively stable over time. These traits affect multiple areas of life, including work, relationships, and self-image.
Common symptoms include:
- Preoccupation with details, rules, lists, and schedules
- Perfectionism that interferes with task completion
- Excessive devotion to work at the expense of leisure and relationships
- Rigid morality, ethics, or values
- Difficulty delegating tasks unless others follow exact rules
- Stinginess toward self and others
Unlike OCD, individuals with OCPD usually believe their way of thinking is correct. This lack of insight can delay diagnosis and treatment.
Treatment
Treatment for OCPD focuses on improving flexibility, emotional awareness, and interpersonal functioning. Because personality traits are deeply ingrained, treatment often requires time and consistent effort.
Psychotherapy is the primary treatment approach. Effective modalities include:
- Cognitive Behavioral Therapy (CBT), which helps challenge rigid beliefs
- Psychodynamic therapy, which explores early experiences and internal conflicts
- Schema therapy, targeting long-standing maladaptive patterns
Medication is not a primary treatment for OCPD but may be prescribed to address coexisting conditions such as depression or anxiety. Selective serotonin reuptake inhibitors (SSRIs) may help reduce rigidity and perfectionism in some individuals.
Successful treatment often depends on the individuals willingness to recognize how their traits affect quality of life and relationships.
Outlook
The long-term outlook for individuals with OCPD varies. While personality traits tend to be stable, meaningful improvement is possible with treatment and self-awareness.
Many individuals learn to balance high standards with flexibility, leading to improved relationships and reduced distress. Progress is often gradual rather than dramatic, but even small changes can significantly improve quality of life.
Early recognition and engagement in therapy are associated with better outcomes.
Support
Support plays a crucial role in managing OCPD. Family members and partners often benefit from education about the condition to better understand behavior patterns.
Helpful support strategies include:
- Encouraging professional help without confrontation
- Setting clear and respectful boundaries
- Practicing open communication
Support groups and psychoeducation resources can also provide reassurance and reduce isolation for both individuals with OCPD and their loved ones.
Frequently Asked Questions about Obsessive-Compulsive Personality Disorder
Is OCPD the same as OCD?
No, OCPD and OCD are different conditions with distinct features.
OCPD involves personality traits, while OCD involves intrusive thoughts and compulsive behaviors.
Can OCPD be cured?
OCPD is not typically cured, but symptoms can improve with treatment.
Therapy can help individuals develop greater flexibility and insight.
Do people with OCPD realize they have a problem?
Many individuals with OCPD believe their behaviors are appropriate or beneficial.
This can make seeking help more challenging.
Can someone with OCPD have healthy relationships?
Yes, healthy relationships are possible with awareness and effort.
Therapy and communication skills play an important role.
How we reviewed this article:
Our team continually monitors and updates articles whenever new information becomes available.
Written By
Ian Nathan, an MBChB Candidate, and the Healtharticles Editorial Team
Medically Reviewed By
Ian Nathan, an MBChB Candidate



